AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
African Research Review: An International
Multidisciplinary Journal, Ethiopia
AFRREV Vol. 14 (1), Serial No 57, January, 2020: 1-16
ISSN 1994-9057 (Print) ISSN 2070-0083 (Online)
DOI: http://dx.doi.org/10.4314/afrrev.v14i1.1
Reducing Old Age Vulnerabilities in Developing Countries: The Role
of Income-Support on Poor Older People’s Health
Awojobi, Oladayo Nathaniel
Department of Social Security
Bonn-Rhein-Sieg University of Applied Sciences
Sankt Augustin, Germany
E-mail: dawojobi@gmail.com
Phone: +4915215820100
Abe, Jane Temidayo
Department of Psychology
Nnamdi Azikiwe University
Awka, Anambra State, Nigeria
E-mail: temidayojabe@gmail.com
Phone: +2348062849579
Abstract
This systematic review is on the impact of income-support on older people’s health in
developing countries. A systematic search for non-randomised and mixed methods studies
published between 2013 and 2017 was conducted in academic and grey literature databases,
websites and references lists of relevant studies. Study methodological quality was assessed
with a risk of bias tool. Inclusion criteria were met by 7 studies, 3 in Latin America, two each
in Africa and Asia. Five of the studies used a quantitative non-randomised approach while the
remaining two used mixed methods analysis. Income-support was discovered to have positive
effects on older people’s nutritional status, cognitive functions, health and psychological
wellbeing. Income-support offers older people access to healthcare services and protection
against detrimental effects of lack of money in accessing healthcare services.
Key Words: Health, income-support, older people
COPYRIGHT © IAARR: https://www.afrrevjo.net
1
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Introduction
The population of older people in developing countries is increasing. For instance, it has been
projected that by the year 2050, the ageing population in sub-Saharan Africa would have
increased to 161 million (Aboderin& Beard, 2015; Audain, Carr, Dikmen, Zotor, &Ellahi,
2017; Nanyonjo, 2016; UN, 2016). Most of the health systems in developing countries are
not prepared adequately for the health demands of older people (HelpAge International,
2017). There are inadequate health facilities specializing on older people’s health as facilities
are not designed to the older people’s medical needs and personnel are not properly trained in
administering care to them (HelpAge International, 2017).
The majority of the older people in developing countries do not have health insurance where
most of the health services are the cash-and-carry systems that mandated patients, even those
brought to the hospital on emergencies to pay cash deposit at every point of service
delivery (HelpAge International, 2017). Also, available data showed that less than 17% of
older people have pensions in sub-Saharan Africa (UN, 2016). Because of this, older people
in the region continue to work on the farms to earn a living (Aboderin& Beard, 2015; UN,
2016). Aside from remaining part of the labour force beyond the stipulated recommended age,
older people in sub-Saharan Africa whose adult children have moved to other cities in search
of work or have died for one reason or the other, also take care of their grandchildren
(Aboderin & Beard, 2015; UN, 2016).
Planning for an ageing population is crucial to the attainment of the integrated 2030 Agenda,
with ageing running across the goals of poverty reduction, good health, economic growth,
gender equality and decent work (Dugarova, 2017). Ghana is one of the leading countries in
sub-Saharan Africa that have taken the initiative to support older people. The government, in
2008, introduced the Livelihood Empowerment Against Poverty (LEAP), a cash transfer
programme for older people of 65 years and above who are considered extremely poor and
live in vulnerable households.
There is increasing empirical evidence pointing to considerable degrees of functional
impairment among older people, partially connected to the protracted disease
burden (Nanyonjo, 2016). It has been reported that older people in developing countries are
prone to a lot of diseases, both communicable and non-communicable ones. Such diseases
include cardiovascular and circulatory disease, cancer, diabetes, cirrhosis of the liver and
nutritional deficiencies (Aboderin& Beard, 2015; Audain et al., 2017; Nanyonjo, 2016; UN,
2016). Furthermore, a survey of older people in Africa showed high levels of “hypertension,
musculoskeletal disease, visual impairment, functional limitations and depression” (Aboderin
& Beard, 2015, p.10). Additionally, contagious illnesses continue to affect older women and
men in sub-Saharan Africa, highlighted by a significant prevalence of HIV infection and its
worsening effect on various non-communicable diseases (Aboderin & Beard, 2015).
Since disease burden increases with age, there is a huge need for the prevention and treatment
of these diseases and long-term care for older people in developing countries (Nanyonjo,
2016; UN, 2016). Studies have shown that older people in developing countries face a
herculean task in accessing healthcare services because of transport cost and the cost of
paying for healthcare services (Aboderin& Beard, 2015; HelpAge International, 2017).
Therefore, social pension interventions or similar interventions for income support to older
people in developing countries are important to the social security of older people (UN,
2016).
COPYRIGHT © IAARR: https://www.afrrevjo.net
2
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/

AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Evidence has shown that income-support plays a crucial role in removing some demand-side
obstacles, such as out-of-pocket expenditures to healthcare for older people (HelpAge
International, 2017). It has also been reported that older people use income-support for
transporting themselves to health facilities, consultation fees and treatment cost as well as
health insurance and prescriptions (HelpAge International, 2017). The general impact of
income-support on older people's health-outcomes in developing countries is not yet fully
known as limited research has been done in this area. For instance, the field of research on
older people's health in sub-Saharan Africa is still at an early stage (Nanyonjo, 2016).
Additionally, limited attention has been given to issues of older people in sub-Saharan Africa,
which remains the earth’s poorest and youngest region (Aboderin& Beard, 2015).
There is the need for a better understanding of the health challenges of older people, their
limited access to health facilities and the crucial role income-support is playing in removing
some demand-side barriers to healthcare services. This review aims to assess the impact of
income-support on older people’s health.
Materials and Methods
Criteria for Considering Studies for the Review
Type of studies
This review aims to assess the impact of income-support on older people’s healthcare. In
order to accomplish the aim of the review, we focused on studies in developing countries that
evaluate the effects of income-support programmes on older people’s health. In a nutshell, we
considered studies that focused on the role of income-support in assisting older people to
access healthcare services. The following study designs were used for the review:
• Quasi experimental design
• Mixed methods
• Cross sectional study
• Quantitative non-randomised
Types of participants
This review included studies that assess the interface between income-support and the health
of older people of the ages of 60 and above in developing economies as defined by the United
Nations (UN, 2014).
Types of interventions
This review included income programmes that were meant to reduce poverty and
vulnerabilities in poor households with older people of 60 years and above. That is, to be
included in this review, interventions must meet the following criteria:
• a non-conditional cash transfer to older people;
• income supplement for poor elderly in low- and middle-income setting;
• old age grants for older people’s wellbeing;
• old age allowance for older people with income not more than USD 35.52 annually;
• social pension to provide minimum income for old age; and
• conditional cash transfer to support vulnerable older people.
Types of outcome measures
COPYRIGHT © IAARR: https://www.afrrevjo.net
3
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
This review included studies that estimated the impact of income-support programmes on
older people’s health and changes in health outcomes. These outcomes are divided into
primary and secondary outcomes measured by the included studies.
Primary outcomes
The following primary outcomes were eligible for the review:
• Use of healthcare services, including but not limited to:
➢ doctor consultation;
➢ outpatient visits;
➢ purchasing of drugs;
➢ transportation cost to healthcare facilities;
➢ treatment of ailments;
➢ use of cash transfers in removing any demand-side barriers to healthcare
services.
• Health outcomes, but not limited to:
➢ cognitive functions;
➢ food security;
➢ improvement in lung functions;
➢ mental wellbeing;
➢ reduction in depressive symptoms.
Secondary outcomes
This review considered the following as the secondary outcomes:
• social determinant of health;
• healthcare expenditure;
• changes in access to healthcare services.
Search Methods for Identification of Studies
We conducted an electronic search for relevant studies for the systematic review. The
searches were conducted in the following databases which included both academic and grey
literature:
• PubMed
• Cochrane Library
• ResearchGate
• African Journals Online
• Google Scholar
• African HealthLine
• HelpAge International Social Pension Database
• Science Direct
• Cambridge Journal Database
• Oxford Journal Database
Aside from the use of electronic search for the selected studies of this review, we searched the
websites of prominent organisations such as the WHO, HelpAge International, World Bank,
USAID and the UK Department of International Development (DFID). We conducted an
COPYRIGHT © IAARR: https://www.afrrevjo.net
4
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
additional search on the reference lists of the included studies in case we have missed any
relevant literature from the electronic search.
Data collection and Analysis
Selection of studies
The two authors were responsible for the selection of relevant studies for the review which
was done independently. The disagreements that emanated from the selection process were
resolved through discussion among the authors. Initially, we screened the titles of the selected
studies and through this process duplicate records were removed. A second round of
screening was done on the titles and abstracts of the selected studies in order to identify
studies that meet the inclusion criteria of the review. An additionally screening of abstracts
and full text of the selected studies paved way for the identification of studies that were
eligible for the review.
Data extraction and management
Data were extracted independently from studies included in this systematic review by the two
authors, (O.A.& J.A.) using the standardised data extraction tool available in JBI SUMARI
(Aromataris& Munn, 2017). Data extracted included the following:
• Author’s names
• Publication date
• Geographical region
• Types of study
• Data collection methods
• Participants
• Interventions
• Main outcome measures and results
Quality assessment
Two authors (O.A and J.A) independently assessed the quality of the included studies. During
this process, the disagreements that emanated were resolved through discussion. To assess
the risk of bias of the included studies, we employed the Mixed Method Appraisal Tool
(MMAT) prepared by (Hong et al., 2018). The risk of bias was assessed by the following
scores: Yes, No and Cannot tell, while the overall appraisal of the risk of bias for the included
studies that was used for the summary assessment were as follow: Include, Exclude, and
Seek further info.
Data synthesis
Due to the heterogeneity in study setting, design, interventions and outcomes mentioned in
the included studies, it was not feasible to statistically combine the results of the studies under
review. In this case, we used qualitative synthesis vis a vis narrative synthesis to present the
estimated effects of income-support on older people’s health from the included studies.
Results
Study Selection
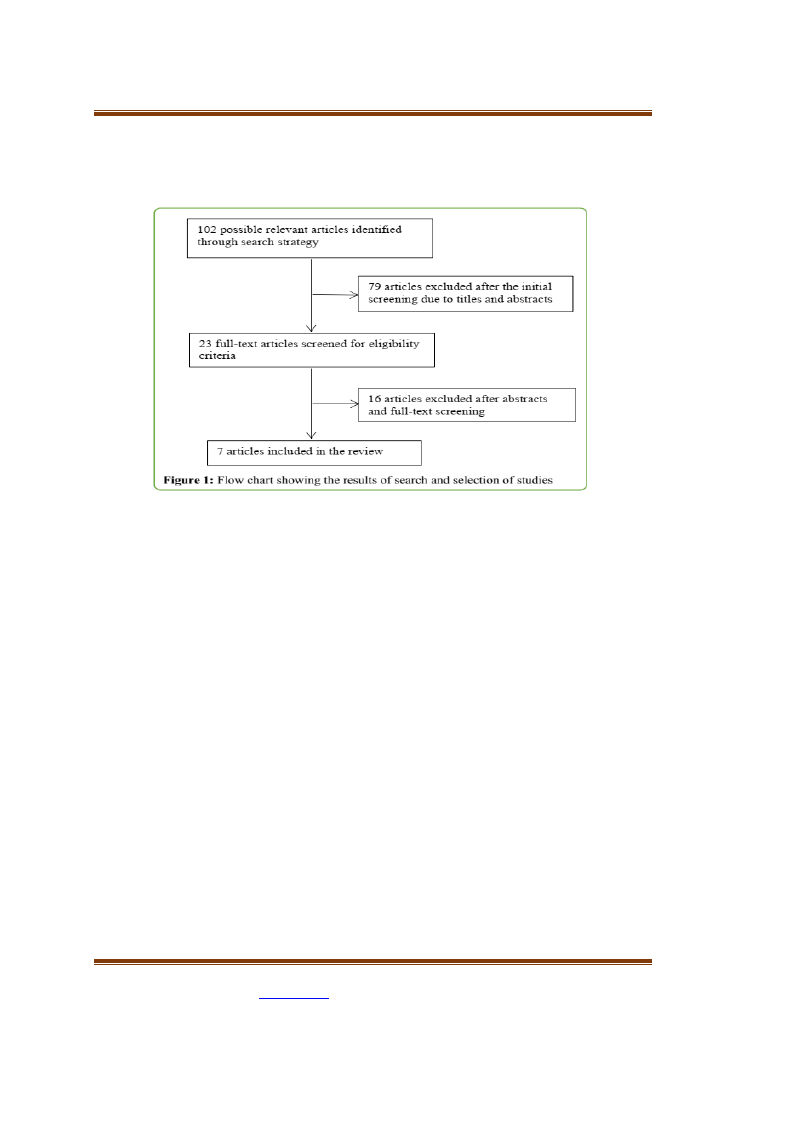
Figure 1 presents the study selection process for the systematic review. Our initial search for
relevant literature produced 102 articles. Due to the screening of titles and abstracts of the
COPYRIGHT © IAARR: https://www.afrrevjo.net
5
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
initial identified articles, 79 articles were excluded, leaving 23 articles for full text screening.
The 23 articles were screened for eligibility through abstracts and full text, leaving only 7
articles for the final review.
Characteristics of the Included Studies
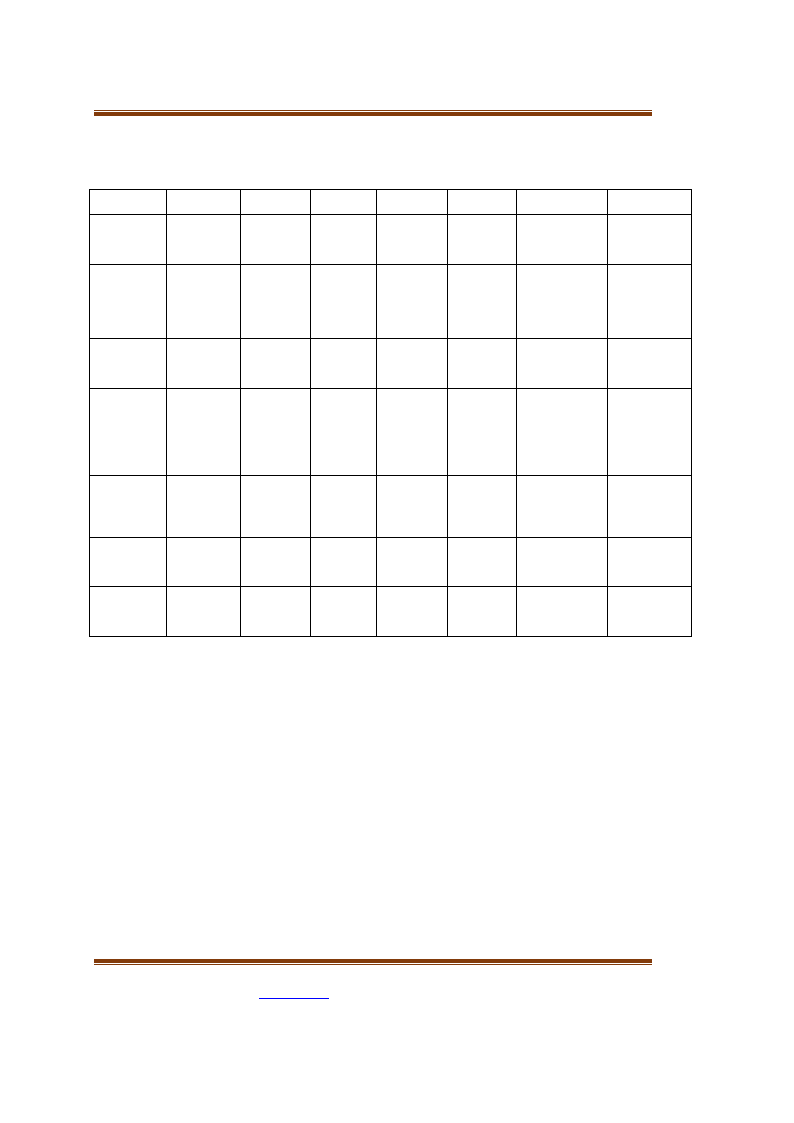
Table 1 shows the characterises of the seven included studies. Geographically, three of the
studies were conducted in Latin America: Mexico (Aguila, Kapteyn, and Smith, 2015;
Salinas-Rodríguez and Manrique-Espinoza, 2013; Salinas-Rodríguez, Torres-Pereda,
Manrique-Espinoza, Moreno-Tamayo, and Téllez-Rojo Solís, 2014); two were conducted in
Asia: Bangladesh (Uddin, 2013) and China (Cheng, Liu, Zhang, and Zhao, 2018); and the
remaining studies were conducted in sub-Saharan Africa: Ethiopia, Mozambique, Tanzania
and Zimbabwe (HelpAge International, 2017) and South Africa (Lloyd-Sherlock and
Agrawal, 2014).
In terms of study design, four studies used non-randomised approach (Aguila et al., 2015;
Cheng et al., 2018; Lloyd-Sherlock and Agrawal, 2014; Salinas-Rodríguez et al., 2014), two
others used mix methods technique (HelpAge International, 2017; Uddin, 2013) and one used
cross sectional (Salinas-Rodríguez and Manrique-Espinoza, 2013). The included study types
composed of four peer-reviewed articles (Aguila et al., 2015; Lloyd-Sherlock Agrawal, 2014;
Salinas-Rodríguez and Manrique-Espinoza, 2013; Salinas-Rodríguez et al., 2014), one
discussion paper (Cheng et al., 2018), one dissertation (Uddin, 2013) and one grey literature
(HelpAge International, 2017).
In terms of intervention, most of the studies focused on cash transfers and social pension.
Data used by the included studies in estimating the effects of income-support on older
people’s health were sourced from different sources such as interview, longitudinal survey
and focus group discussion. Outcomes measured by the included studies include health
benefits, physical health, mental health, vaccination and access to healthcare services.
COPYRIGHT © IAARR: https://www.afrrevjo.net
6
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Table 1: Characteristics of the includedstudies
Authors
Date
Aguila et al.
(2014)
Cheng et al.
(2016)
HelpAge
International
(2017)
Lloyd-
Sherlock and
Agrawal
(2014)
Salinas-
Rodríguez and
Manrique-
Espinoza
(2013)
Salinas-
Rodríguez et
al.(2014)
Uddin (2013)
Country
Mexico
China
Ethiopia,
Mozambique,
Tanzania and
Zimbabwe
South Africa
Mexico
Mexico
Bangladesh
Study
design
Quasi-
experimental
Non-
randomised
Mixed
methods
Non-
randomised
Cross-
sectional
Non-
randomised
Mixed
methods
Type of
study
Peer-
reviewed
Discussion
paper
Grey
literature
Peer-
reviewed
Peer-
reviewed
Peer-
reviewed
Dissertation
Intervention
Income
supplement
Social
pension
Cash
transfers
Social
pension
Conditional
cash transfer
Non-
contributory
social
pension
Old-age
allowance
Participant
Seventy-
year and
above
Elderly
population
aged 60 and
above
158 elderly
people
Black
African
women aged
60 and over
and men
aged 63 and
over
12,146 older
people
5,270 older
adults
40
programme
beneficiaries
Data source
Rich data
capturing health
and wellbeing in
old age
Chinese
Longitudinal
Healthy
Longevity
Survey
(CLHLS)
Focus group
discussion,
interview
World Health
Organization
(WHO) survey of
Global Ageing
and Adult Health
(SAGE)
2007
Oportunidades
Evaluation
Survey
Baseline and
follow-up survey
Data from
primary and
secondary
sources
Outcomes
measured
Health benefits
Physical health,
cognitive
function, and
psychological
well-being
Access to
healthcare
services
Health service
utilisation,
hypertension
awareness and
treatment
Vaccination
coverage
Mental
wellbeing
Access to
healthcare
facilities
Methodological Quality of Included Studies
We used MMAT risk of bias tool to assess the methodological quality of the included studies
(Hong et al.,). The quality of the five quantitative studies included in the review was high
because each of the study scored the following grades 5/5; (Lloyd-Sherlock and Agrawal,
2014); 4/5 each for (Aguila, Kapteyn, & Smith, 2015; Cheng et al., 2018; Salinas-Rodríguez
and Manrique-Espinoza, 2013; Salinas-Rodríguez et al., 2014) from the methodological
quality criteria. All the study measurements were appropriate for both their outcomes and
interventions and their study participants were representative of the target population.
The quality of two of the mixed method studies was moderate, as each of the study scored 3/5
(HelpAge International, 2017; Uddin, 2013) from the methodological quality criteria. The two
studies showed adequate rationale for using mix methods design to address the research
question. The different components of the studies were adequately integrated to answer the
research question and the outputs of the combination of the qualitative and quantitative
components were effectively interpreted.
COPYRIGHT © IAARR: https://www.afrrevjo.net
7
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Effects of Interventions
Impact on Anthropometric or Nutritional Outcomes
Of the seven studies we reviewed, three reported on the role of income-support programmes
on poor older people’s anthropometric or nutritional status (Aguila et al., 2015; Cheng et al.,
2018; HelpAge International, 2017). In China, social pension enrolment had positive and
significant impact on older people’s height as they experienced 3.5 cm less height shrinkage
than poor older people not receiving social pensions (Cheng et al., 2018). Similarly, a 100
percent rise in pension income had a significant effect on height loss reduction by 0.8 cm
(Cheng et al., 2018). In sum, the social pensions had a positive effect on the physical health of
older people (Cheng et al., 2018). In Ethiopia, cash transfers improved nutrition and food
security for older people (HelpAge International, 2017). According to one of the female
respondents from the focus group discussion:
We used to have one or two meals but now we have three meals. We are also
able to buy vegetables and onions and buy meat twice a month to vary the
diet. We can also buy soap to wash our clothes and utensils and wash clothes
for our children and grandchildren. I feel stronger and more energetic than
before... I am sure I even look more beautiful(HelpAge International, 2017,
p. 23).
In Mexico, income supplementation on the health of poor older people showed that little
segment of the older people receiving income supplement reported that they ran out of food
stuff in the last three months compared to poor older people not receiving income
supplementation (Aguila et al., 2015). In addition, the treatment group reported a significant
decrease of being hungry and not eating all day compared to the control group (Aguila et al.,
2015).
Impact on Cognitive Functions
Two studies of the seven studies we reviewed reported on the interface between income-
support and older people’s cognitive functions (Aguila et al., 2015; Cheng et al., 2018). In
China, the take-up of social pensions had a positive effect on the cognitive functions of older
people (Cheng et al., 2018). The findings of the study revealed that enrolment in the pension
programme significantly improved Mini-Mental State Examination (MMSE) score by more
than 2 points and raised the probability of excellent cognitive function by 18 percentage
points (Cheng et al., 2018). Additionally, a 100 percent increase on the social pension benefits
led to a 0.57-point rise in MMSE score, 4.2 percentage points more beneficiaries having
excellent cognitive function (Cheng et al., 2018).
In Mexico, the study of Aguila et al. (2015), using DID estimates to carry simple exercise on
older people’s cognitive function showed that they regressed the health conditions on age and
age squared taking cognisance of peak flow, immediate and delayed recall. Their findings
revealed a marked reduction with age. In continuation of their analysis, they interviewed a 78-
year-old individual in their study sample to know if the income supplement enhances his
health and how much younger the older individual has to be to enjoy the same level of health
in the case of no income supplement. Their findings showed that improvement in immediate
recall was the same as if the study individual were about 5.5 years younger. In the case of
delayed recall, the improvement was tantamount to being 12.4 years younger. For peak flow,
the improvement was commensurate to being 7 years younger (Aguila et al., 2015).
COPYRIGHT © IAARR: https://www.afrrevjo.net
8
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Impact on Health Outcomes
Four studies reported health outcomes due to cash transfers on older people (Aguila, Kapteyn,
and Smith, 2015; Cheng et al., 2018; HelpAge International, 2017; Lloyd-Sherlock and
Agrawal, 2014). In China, social pension enrolment by older people led to a significant
reduction in the incidences of hypertension by 21 percentage points and enhanced their
instrumental activities of daily living (IADL) performance by 11 percentage points (Cheng et
al., 2018). Additionally, a 100-percent rise in pension income significantly reduced the
probability of experiencing hypertension by 5.4 percentage points and significantly enhanced
the probability of performing IADL by 2.4 percentage points (Cheng et al., 2018). However,
both the enrolment and increase in pension income by older people have no significant effect
on self-reported general health (Cheng et al., 2018).
The study that investigated the impact of cash transfers on older people’s access to healthcare
services in Ethiopia, Mozambique, Tanzania and Zimbabwe revealed that older people in
these countries faced obstacles in accessing healthcare services because of their economic
conditions. Aside from this, the older people in the study sample from the four countries
reported being affected by non-communicable diseases such as arthritis (Ethiopia 40%;
Mozambique 75%; Tanzania 33%; Zimbabwe 21%); asthma (Ethiopia 11%; Mozambique
12%; Tanzania 9%; Zimbabwe N/A); diabetes (Ethiopia 10%; Mozambique N/A; Tanzania
10%; Zimbabwe 5%); eye problems (Ethiopia 30%; Mozambique 38%; Tanzania 39%;
Zimbabwe 15%); and hypertension (Ethiopia 20%; Mozambique 40%; Tanzania 29%;
Zimbabwe 16%) (HelpAge International, 2017). Despite the cash transfers being recognised
as not being enough to meet the health needs of older people, they were successful in
improving the older people’s abilities to identify and act on their health needs because they
were associated with health awareness activities in Ethiopia and Tanzania (HelpAge
International, 2017).
In Mexico, empirical evidence showed that older people living in Yucatan who received
income supplement had a statistically significant improvement in both immediate and delayed
recall coupled with improvement in lung function measured by peak flow (Aguila et al.,
2015). Additionally, the income supplement helped poor older beneficiaries to have little
presence of low haemoglobin levels linked to fatigue. This effect was marginally significant
to the conventional P value but not significant when Holm-Bonferroni correction was applied
(Audain et al., 2017). In South Africa, poor black older people receiving social pension had a
significant pension status associated with awareness of hypertensive status (OR:2.80; 95%
CI:1.68-4.67), but rural setting was significantly associated with lower awareness (0.61; 95%
CI:0.45-0.82) (Lloyd-Sherlock and Agrawal, 2014)
Impact on Psychological Wellbeing
Three studies reported outcomes on psychological wellness for poor older people after
receiving cash income-support (Cheng et al., 2018; HelpAge International, 2017; Salinas-
Rodríguez et al., 2014). The results obtained in China showed that social pension uptake had
negative and statistically significant result for depression index while a 100-percent increase
in pension income had 0.30 percentage points reduction in depression index (Cheng et al.,
2018). These indicated that the social pension has improved the psychological wellbeing of
the poor older people receiving it (Cheng et al., 2018). The analysis of cash transfer
programmes in Ethiopia, Mozambique, Tanzania and Zimbabwe showed positive effects
despite the little amount of cash receipts given to poor older people (HelpAge International,
COPYRIGHT © IAARR: https://www.afrrevjo.net
9
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
2017). Evidence showed significant effects of cash transfers allowing older people to better
meet their basic needs, especially in buying different types of food stuff, and hygiene
products. Participants of the focus group discussions in the four countries reported that a large
amount of their cash transfers were spent on food and soap. In Mozambique, cash transfers
were spent in accessing potable water (Salinas-Rodríguez et al., 2014). According to one of
the key informants interviewed in Ethiopia: “Cash transfers also improve the psychology and
self-esteem of the family and the elderly people in particular – the more they secure their
livelihoods, the more they are socially included”(HelpAge International, 2017, p. 23).
The evaluation of Mexican non-contributory social pension scheme showed that after one-year
exposure to the scheme, the beneficiaries’ depressive symptoms significantly decreased (β =
20.06, CI95% 20.12; 20.01) (Salinas-Rodríguez et al., 2014). Similarly, the social intervention
contributed to higher feelings of safety and welfare linked with reduced depressive symptoms
among poor older people (Salinas-Rodríguez et al., 2014). According to some of the
statements of the old beneficiaries of the social intervention, they experienced a decrease or
relief of poverty and stress associated with lack of income and an expanded sense of social
security and wellbeing from receiving monthly income that they could regard their own and
on which they can decide what to do (Salinas-Rodríguez et al., 2014). One of the older
recipients of the social intervention stated:
Now I eat better, now I have ‘a cent’ to buy at least a piece of meat,
something like that… some bread. Before, it was not like this. we couldn’t
buy anything because we did not have money (laughter), and now, yes now,
we have this. I do feel better (Salinas-Rodríguez et al., 2014, p. 6).
Impact on Uptake of Healthcare Services
Six studies reported on the uptake of healthcare services by poor older people due to cash
transfer in their possession (Aguila et al., 2015; HelpAge International, 2017; Lloyd-Sherlock
and Agrawal, 2014; Salinas-Rodríguez and Manrique-Espinoza, 2013; Salinas-Rodríguez et
al., 2014; Uddin, 2013). In Bangladesh, a mixed-method analysis showed that prior to the
introduction of old age allowance, poor older people access healthcare services through the
support of their family members (Uddin, 2013). However, with the introduction of the old age
allowance, 97.5% of the study sample purchased their necessary drugs from their allowance
(Uddin, 2013). This showed from the study’s findings that 94.87% of the poor older people
had met their essential medication with the aid of the allowance (Uddin, 2013).
The impact evaluation of HelpAge International on cash transfers and older people’s access to
healthcare services in four sub-Saharan African countries showed that cash transfer
programmes helped poor older people to access healthcare services (HelpAge International,
2017). The older people in these four countries identified the cost of transportation to health
facilities as hindrance in accessing healthcare services (HelpAge International, 2017).
However, with the cash transfer programmes, most of the beneficiaries were able to access
healthcare services. In Ethiopia, one of the beneficiaries stated: “Through the cash transfer, I
have money for transport to go and seek healthcare services” (HelpAge International, 2017,
p. 21). While in Tanzania, an old recipient of the cash receipt had this to say: “Sometimes
when [the cash transfer] is there, it helps to meet transport costs to the hospital. If the cash
transfer money is there I do not beg – I just use it to go to the health facility”(HelpAge
International, 2017, p. 21)
COPYRIGHT © IAARR: https://www.afrrevjo.net
10
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Aside from the use of cash transfers in paying for transport cost to health facilities, older
people in the impact evaluation analysis use cash transfers to pay for hospital bills, treatment
and medicines. In Ethiopia, a male respondent stated: “Without the cash transfer, we would
not be able to access any health services as they are too expensive, even at the health
centre”(HelpAge International, 2017:21). In Mozambique, the cash transfers helped an old
male patient to pay for his medical surgery. According to him:“I had an operation and the
money from the PSSB helped to pay for it”(HelpAge International, 2017, p. 22).
The difference-in-difference estimates in Mexico on the effects of income supplementation on
the health of older people showed that the intervention supported half of the beneficiaries’
visit to a doctor and the number of visits to doctors increased compared to those of non-
beneficiaries (Aguila, Kapteyn, & Smith, 2015). The monthly cash received by the older
people gave a sense of relief to their relatives who were responsible for out-of-pocket (OOP)
spending on healthcare services. The income support helped the older people to pay for their
healthcare expenditure. However, some of them complained of the high cost of drugs (Aguila
et al., 2015). In a similar study also in Mexico, vaccination coverage among cash transfer
beneficiaries and non-beneficiaries stood at 46% and 41% for influenza, 52% and 45% for
pneumococcal disease and 79% and 71% for tetanus respectively. The study analysis showed
that the cash transfer programme exerted a significant impact on immunisation and had an
effect of 0.069 (CI95%: 0.038, 0.096; p < 0.001) on influenza vaccine. Further analysis of the
study revealed that “pneumococcal and tetanus vaccine results were analogous with
coefficient value of 0.0.72 (CI95%: 0.043, 0.102; p <0.001) and 0.066 (CI95%: 0.041, 0.092,
p <0.001), respectively” (Salinas-Rodríguez and Manrique-Espinoza, 2013, p. 5)
Aside from the cash transfer programme making influenza immunisation coverage 7% higher
for beneficiaries of the intervention than those of non-beneficiaries, the intervention increased
the possibility of taking up the complete vaccination schedule (coefficient = 0.055, CI95%:
0.028, 0.028; p < 0.001) (Salinas-Rodríguez & Manrique-Espinoza, 2013).
In the Mexican State of Yucatan, a qualitative interview showed that before the introduction of
non-contributory social pension, one of the beneficiaries of the intervention felt unhappy for
not having money to access healthcare services. However, with the introduction of the
intervention, he was happy for receiving the intervention:
Well, indeed I did not feel sad. I was ashamed because the money was not
enough to buy needed things, and then, when I got sick, I used to have to beg
for money. But now, at least we have some money. If I get sick, at least I
have money to buy medicine that [the health services] don’t have(Salinas-
Rodríguez et al., 2014, p. 6)
In South Africa, the study conducted by Lloyd-Sherlock and Agrawal (2014), on cash
transfers and older people’s health showed mixed effects. The cash transfer programme was
significantly linked with more frequent outpatient visits for beneficiaries of the programme
(OR 1.77; 95% CI1.00-3.15). However, the analysis of the programme did show that rural
setting was not significantly linked with outpatient visits. Nevertheless, the programme was
significantly associated with lower awareness (OR:0.61: 95% ci:0.45-0.82) and the treatment
of hypertension (OR:0.68; 95% CI: 0.49-0.94). On older female beneficiaries, the programme
was associated with healthcare utilisation (OR:1.56; 95% CI: 1.15-2.12), awareness (OR:1.95;
95% CI:1.44-2.64) and treatment (OR:1.86; 95% CI: 1.35-2.57) (Lloyd-Sherlock and
Agrawal, 2014).
COPYRIGHT © IAARR: https://www.afrrevjo.net
11
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Discussion
This review is the first to assess the impact of income-support for older people’s health in
developing countries. The findings from the systematic review showed that income-support to
older people helped in improving their anthropometric or nutritional status, cognitive
functions and psychological wellbeing. In addition, income-support allows older people to
access health services which in turn improve their health status.
Income inequality prevents people from both developed and developing countries from
accessing health services when needed. For instance, in the British Columbia, Canada, it was
discovered that people with lower incomes were less likely to access general practitioner (GP)
and specialist services (Penning and Zheng, 2016). In sub-Sahara Africa, studies have shown
that poverty hinders children, women and the vulnerable from accessing healthcare service
when they are indisposed (Aregbeshola& Khan, 2018; Awiti, 2014; Keya et al., 2018; Lanre-
Abass, 2008). Older people are the ones mostly affected by poverty in developing countries,
especially older people without social security or pension benefits (Marmot, 2006). The
prevalence of poverty among older people in developing countries has been responsible for
many governments’ use of income-support for older people.
Our findings showed that income-support improved older people’s anthropometric or
nutritional status in China, Ethiopia and Mexico. Although it had a significant effect in China,
the study did not have the same significant level of effect in Ethiopia, while in Mexico, it had
no significant effect. Nevertheless, there was a significant effect on food security for
beneficiaries of the intervention than non-beneficiaries.
In terms of cognitive functions, only two studies reported positive effects: those in China and
Mexico. While in Mexico, the studies did not present the outcomes of the intervention on the
study sample, it, however, stated that the intervention had a significant impact on a subgroup.
It was possible for the study in China to assess the cognitive functions of older beneficiaries of
the social pension programme through MMSE score. Those who enrolled in the social pension
programme had a 100% increase in income benefit and the income benefit improved their
MMSE score with a significant effect. Income- support has been known to improve the
cognitive functions of beneficiaries through the consumption of variety of diets. In Nicaragua,
beneficiaries that were exposed to cash transfer programme had their cognitive development
raised by 0.09 standard deviations compared to the non-beneficiary group in 2006, and 0.08
standard deviations greater in 2008 (Macours et al., 2012).
Findings from this review also showed that income-support improve the health outcomes and
psychological wellbeing of older people. Data from the three studies that evaluated income-
support and the wellbeing of older people in China, Ethiopia and Mexico revealed that the
beneficiaries of the interventions felt happy because the income-support added value to their
life. Similar studies have revealed the estimated positive effects of income-support on the
wellbeing of beneficiaries in Columbia, Ghana, Kenya and Lesotho (Attah et al., 2016;
Martínez & Maia, 2018; Pereira, 2016).
Aside from the evidence from this review on the positive effects of income-support on the
psychological wellbeing of older people, our findings also showed positive effects of income-
support on older people’s health. From our review, income-support had positive effects on
hypertension awareness, allowed beneficiaries to identify and act on their health needs, and a
reduction in the incidences of hypertension and improved lung functions. However, one study
reported no effect of income-support on self-reported general health in China. Two studies
COPYRIGHT © IAARR: https://www.afrrevjo.net
12
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
that used systematic reviews to assess the impact of cash transfers on health outcomes showed
strong evidence of cash transfer uptake on the health outcomes of beneficiaries of the
programmes (Lagarde et al., 2009; Pega et al., 2017).
Among the seven studies we reviewed, six assessed the impact of income-support on the
uptake of healthcare services by older people. Our findings showed that income-support
enhanced the uptake of healthcare services when needed. Income-support helped older people
to transport themselves to health facilities, pay for medical services, including the purchase of
medical drugs. Aside from these, one beneficiary was able to use the income-support to pay
for surgery. In Ethiopia, Mozambique, Tanzania and Zimbabwe, the beneficiaries of the
income-support programmes agreed that the income they received was little, but most of them
were able to use the little income to access healthcare services. Similar studies have been able
to prove the positive effects of income support on the uptake of healthcare services (see
Lagarde et al., 2009; Pega et al., 2017).
Our findings have been able to prove the positive effects of income-support on the health of
older people in developing countries. These findings are in consonance with the findings of
similar studies in the United States. Data provided by the Gregory Armstrong of the Centres of
Disease Control and Prevention (CDC) in the study of Arno et al (2011), supported their
hypothesis that income-support programme had a beneficial impact on the health of older
people in the United States. In a similar vein, an income-support programme, Earned Income
Tax Credit (EITC), was reported to have had a positive impact on the health of Americans
(Arno et al.,2009).
There are some limitations that this review encountered. Firstly, because older people face a
lot of challenges, especially in developing countries where there are limited social protection
schemes to support them, data on the impact of income-support on older people’s health were
very scarce. Consequently, of the selected studies for this review, only seven met our inclusion
criteria. Secondly, our search for relevant literature was limited to studies conducted in
English; whereas, there are various studies on social protection for the elderly in Latin
America conducted in other languages. Finally, in some of the studies included in this review,
we discovered missing data that might have been helpful in our analysis.
Conclusion
This systematic review is the first to assess the impact of income-support on older people’s
health in developing countries. Our analysis showed that income-support to poor older people
improved their health and wellbeing. Although income-support are meant to support older
people in various aspect of their lives, our analyses was limited to older people’s health.
The limitations of this review make it mandatory for further research on the subject area.
Nevertheless, our findings have implications for healthcare policies in developing countries. It
has been proved that income inequality hinder access to healthcare services among the
vulnerable. Governments in developing countries need the political will to design and
implement social health insurance programmes that will have access to healthcare service to
all irrespective of socioeconomic status.
Our systematic review findings have shown that social protection mechanisms address the
exclusion and vulnerability of older people. This current evidence supports the relevance of a
life-course mechanism to ageing and the calls for improving and protecting older people
against social exclusion in the implementation of SDGs.
COPYRIGHT © IAARR: https://www.afrrevjo.net
13
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
References
Aboderin, I. A. G., & Beard, J. R. (2015). Older people’s health in sub-Saharan Africa. The
Lancet, 385(9968), e9–e11. https://doi.org/10.1016/S0140-6736(14)61602-0
Aguila, E., Kapteyn, A., & Smith, J. P. (2015). Effects of income supplementation on health
of the poor elderly: The case of Mexico. Proceedings of the National Academy of
Sciences of the United States of America, 112(1), 70–75.
https://doi.org/10.1073/pnas.1414453112
Aregbeshola, B. S., & Khan, S. M. (2018). Out-of-pocket payments, Catastrophic health
expenditure and poverty among households in Nigeria 2010. International Journal of
Health
Policy
and
Management,
7(9),
798–806.
https://doi.org/10.15171/ijhpm.2018.19
Arno, P. S., House, J. S., Viola, D., & Schechter, C. (2011). Social security and mortality:
The role of income support policies and population health in the United States.
Journal of Public Health Policy, 32(2), 234–250. https://doi.org/10.1057/jphp.2011.2
Arno, P. S., Sohler, N., Viola, D., & Schechter, C. (2009). Bringing health and social policy
together: The case of the earned income tax credit. Journal of Public Health Policy,
30(2), 198–207. https://doi.org/10.1057/jphp.2009.3
Aromataris, E., & Munn, Z. (Eds.) (2017). Chapter 1: JBI systematic reviews. Retrieved 23
October
2019,
from
https://wiki.joannabriggs.org/display/MANUAL/Chapter+1%3A+JBI+Systematic+R
eviews
Attah, R., Barca, V., Kardan, A., MacAuslan, I., Merttens, F., & Pellerano, L. (2016). Cash
transfers and psychosocial well-being: Evidence from four African countries (No.
333). Retrieved from International Policy Centre for Inclusive Growth website:
https://ideas.repec.org/p/ipc/opager/333.html
Audain, K., Carr, M., Dikmen, D., Zotor, F., & Ellahi, B. (2017). Exploring the health status
of older persons in Sub-Saharan Africa. The Proceedings of the Nutrition Society,
76(4), 574–579. https://doi.org/10.1017/S0029665117000398
Awiti, J. O. (2014). Poverty and health care demand in Kenya. BMC Health Services
Research, 14. https://doi.org/10.1186/s12913-014-0560-y
Cheng, L., Liu, H., Zhang, Y., & Zhao, Z. (2018). The health implications of social pensions:
Evidence from China’s new rural pension scheme. Journal of Comparative
Economics, 46(1), 53–77. https://doi.org/10.1016/j.jce.2016.12.002
Dugarova, E. (2017). Ageing, older persons and the 2030 Agenda for Sustainable
Development. UNDP.
COPYRIGHT © IAARR: https://www.afrrevjo.net
14
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
HelpAge International. (2017). Cash transfers and older people’s access to healthcare: A
multicounty study in Ethiopia, Mozambique, Tanzania and Zimbabwe. Retrieved from
http://www.helpage.es/silo/files/cash-transfers--.pdf
Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., … Vedel, I.
(2018). Mixed Methods Appraisal Tool (MMAT) VERSION 2018. McGill University,
Department of Family Medicine.
Keya, K. T., Sripad, P., Nwala, E., & Warren, C. E. (2018). ‘Poverty is the big thing’:
Exploring financial, transportation, and opportunity costs associated with fistula
management and repair in Nigeria and Uganda. International Journal for Equity in
Health, 17(1), 70. https://doi.org/10.1186/s12939-018-0777-1
Lagarde, M., Haines, A., & Palmer, N. (2009). The impact of conditional cash transfers on
health outcomes and use of health services in low- and middle-income countries.
Cochrane
Database
of
Systematic
Reviews.
https://doi.org/10.1002/14651858.CD008137
Lanre-Abass, B. A. (2008). Poverty and maternal mortality in Nigeria: Towards a more viable
ethics of modern medical practice. International Journal for Equity in Health, 7, 11.
https://doi.org/10.1186/1475-9276-7-11
Lloyd-Sherlock, P., & Agrawal, S. (2014). Pensions and the health of older people in South
Africa: Is there an effect? The Journal of Development Studies, 50(11), 1570–1586.
https://doi.org/10.1080/00220388.2014.936399
Macours, K., Schady, N., & Vakis, R. (2012). Cash transfers, behavioral changes, and
cognitive development in early childhood: Evidence from a randomized experiment.
Applied Economics, 4(2), 27.
Marmot. (2006). Health in an unequal world. Lancet (London, England), 368(9552), 2081–
2094. https://doi.org/10.1016/S0140-6736(06)69746-8
Martínez, D. M., & Maia, A. G. (2018). The impacts of cash transfers on subjective wellbeing
and poverty: The case of Colombia. Journal of Family and Economic Issues, 39(4),
616–633. https://doi.org/10.1007/s10834-018-9585-4
Nanyonjo, A. (2016, December 16). Long Term care systems for older adults in sub-Saharan
Africa: Are new approaches needed? Retrieved 22 October 2019, from IHP website:
https://www.internationalhealthpolicies.org/blogs/long-term-care-systems-for-older-
adults-in-sub-saharan-africa-are-new-approaches-needed/
Pega, F., Liu, S. Y., Walter, S., Pabayo, R., Saith, R., & Lhachimi, S. K. (2017).
Unconditional cash transfers for reducing poverty and vulnerabilities: Effect on use of
health services and health outcomes in low- and middle-income countries. Cochrane
Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD011135.pub2
COPYRIGHT © IAARR: https://www.afrrevjo.net
15
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
AFRREV VOL 14 (1), S/NO 57, JANUARY, 2020
Penning, M. J., & Zheng, C. (2016). Income inequities in health care utilization among Adults
aged 50 and older. Canadian Journal on Aging = La Revue Canadienne Du
Vieillissement, 35(1), 55–69. https://doi.org/10.1017/S0714980815000562
Pereira, A. (2016). Cash transfers improve the mental health and well-being of youth:
Evidence from the Kenyan cash transfer for orphans and vulnerable children.
UNICEF.
Salinas-Rodríguez, A., & Manrique-Espinoza, B. S. (2013). Effect of the conditional cash
transfer program Oportunidades on vaccination coverage in older Mexican people.
BMC International Health and Human Rights, 13, 30. https://doi.org/10.1186/1472-
698X-13-30
Salinas-Rodríguez, A., Torres-Pereda, Ma. D. P., Manrique-Espinoza, B., Moreno-Tamayo,
K., andTéllez-Rojo Solís, M. M. (2014). Impact of the non-contributory social
pension Program 70 y más on Older Adults’ Mental Well-Being. PLoS ONE, 9(11).
https://doi.org/10.1371/journal.pone.0113085
Uddin, A. (2013). Social safety nets in Bangladesh: An analysis of impact of old age
allowance
program
(BRAC
University).
Retrieved
from
https://core.ac.uk/download/pdf/61804718.pdf
United Nations. (2014). World economic situation and prospects. Retrieved from
https://www.un.org/en/development/desa/policy/wesp/wesp_current/2014wesp_count
ry_classification.pdf
United Nations. (2016). Sub-Saharan Africa’s growing population of older persons. Retrieved
from
https://www.un.org/en/development/desa/population/publications/pdf/popfacts/PopFa
cts_2016-1.pdf
COPYRIGHT © IAARR: https://www.afrrevjo.net
16
Indexed African Journals Online: www.ajol.info
Indexed Society of African Journals Editors (SAJE); https://africaneditors.org/
